Aging U.S. immigrant population poses challenges to state health care systems
Research team by UCLA finds that better access to insurance for aging immigrants would improve access to health care & reduce emergency room costs.
A team led by Dr. Arturo Vargas Bustamante, UCLA Fielding School of Public Health professor of health policy and management and director of faculty research at the UCLA Latino Policy and Politics Initiative (LPPI), has found the United States faces a potential crisis in terms of health care for documented, and undocumented immigrants.
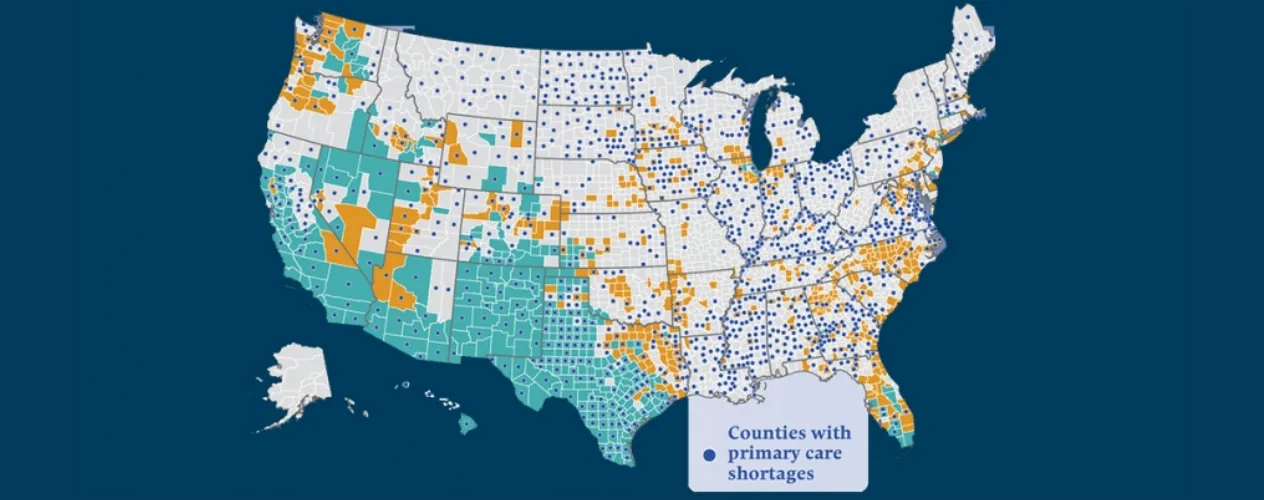
“If present trends continue, the health system will face an increasing population of aging immigrants, of whom many are ineligible for either Medicare or Medicaid,” said Bustamante, an economist who focuses on health policy. “Even though emergency treatment is available to all immigrants—regardless of their documentation status—under the Emergency Medical Treatment and Labor Act, this type of coverage discourages primary care in favor of emergency department care, which is more costly for users and taxpayers.”
The study - Health Policy Challenges Posed by Shifting Demographics and Health Trends among Immigrants to the United States – is being published in the July issue of the peer-reviewed journal Health Affairs. Bustamante’s co-authors include researchers from the University of Maryland, Drexel University, and UCLA. In addition, Bustamante served as editorial advisor for the entire issue.
The U.S. health care system is largely unprepared to deal with aging immigrants, particularly those who are uninsured and live in states where they cannot receive Medicaid, as well as undocumented immigrants who are ineligible for Medicare, according to the research published in Health Affairs. This shifts the need to care for this population to state and local safety-net providers.
Because comprehensive immigration reform in Congress is unlikely, researchers argue for more incremental approaches that increase coverage to underserved aging immigrants. One option could expand health care to aging undocumented immigrants, similar to California’s legislature considering expanding Medicaid coverage for low-income undocumented immigrants ages 65 and older. Another option is Illinois’ coverage of end-stage kidney disease for undocumented immigrants.
The upcoming issue – to be published July 6 - focuses on borders, immigrants, and health. It was written and edited by an interdisciplinary team of physicians, researchers, and economists, and is designed to provide background for public policy makers in both the United States and Mexico.
“About one in seven residents of the U.S. is an immigrant, and about 15 million people live within 60 miles of the U.S.-Mexico border,” said Alan R. Weil, editor-in-chief of Health Affairs. “Disparities in health status exist between people born in the U.S., and those who have immigrated, and current policies in the U.S. and Mexico have significant effects on the health and well-being of tens of millions of people.”
In turn, how this population receives medical care has a significant impact on the economies and budgets of both nations, the researchers said. Overall, the analysis by Bustamante’s team found the U.S. health care system is largely unprepared to deal with aging immigrants, particularly those who are uninsured and live in states where they cannot receive Medicaid, as well as undocumented immigrants who are ineligible for Medicare.
“Access to affordable health insurance would help protect immigrant household incomes and encourage optimal access to and use of health care,” Bustamante said. “And, ultimately, this would provide far more cost-effective, and efficient, healthcare, and would use what funds are available in a far less costly way.”
Other pieces in the edition focus on related issues, including:
- Chilling Effects: US Immigration Enforcement and Health Care Seeking Among Hispanic Adults; Abigail S. Friedman of the Yale School of Public Health and Atheendar S. Venkataramani of the University of Pennsylvania.
- Noncitizen Children Face Higher Health Harms Compared With Their Siblings Who Have US Citizen Status; Mariellen Jewers and Leighton Ku of George Washington University.
- Health Insurance Coverage in Mexico among Return Migrants: Differences between Voluntary Return Migrants and Deportees; Arturo Vargas Bustamante and Rodrigo Dominguez Villegas of the University of California, Los Angeles.
- Understanding The Health Landscapes Where Latinx Immigrants Establish Residence in the US; Elizabeth Ackert of University of California, Santa Barbara and coauthors.
- Health Care Spending and Use Among Hispanic Adults With and Without Limited English Proficiency, 1999–2018; Jessica Himmelstein and coauthors of Cambridge Health Alliance.
- In-Transit Migrants and Asylum Seekers: Inclusion Gaps in Mexico’s COVID-19 Health Policy Response; Ietza Bojorquez-Chapela of El Colegio de la Frontera Norte in Tijuana, Mexico, and coauthors.
- Health Insurance Access among US Citizen Children in Mexico: National and Transborder Policy Implications; Sharon Borja of the University of Houston, and coauthors.
For more information on the analyses by Bustamante and UCLA faculty, including the articles, methods, data sources, and funding, contact Brad Smith at the UCLA Fielding School. In addition, Bustamante will serve as a panelist in two public discussions of this work:
July 12, 2021 - Health Affairs Briefing: Border Health: Evidence & Policy
July 20, 2021 - Health Affairs Briefing: Immigrant Health: Evidence & Policy
For more information on these events, and the other research presented in the July edition, contact:
Sue Ducat, Health Affairs
(202) 361-5115