UCLA FSPH Public Health Magazine
Bringing readers to the forefront of topical public health issues with information and insights from renowned researchers, exploring solutions from origin to impact, and more.
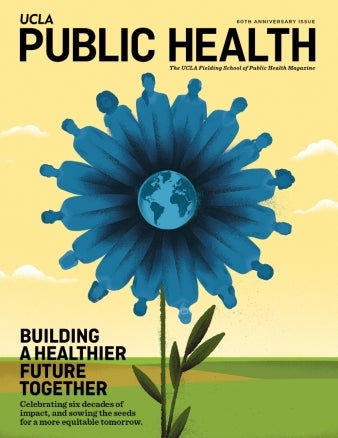
60th Anniversary Issue
Building a Healthier Future Together
Celebrating six decades of impact, and sowing the seeds for a more equitable tomorrow.
Read Full Issue