Mistrust of government often deters older adults from HIV testing

One out of every four people living with HIV/AIDS is 50 or older, yet these older individuals are far more likely to be diagnosed when they are already in the later stages of infection. Such late diagnoses put their health, and the health of others, at greater risk than would have been the case with earlier detection.
According to the Centers for Disease Control and Prevention, 43 percent of HIV-positive people between the ages of 50 and 55, and 51 percent of those 65 or older, develop full-blown AIDS within a year of their diagnosis, and these older adults account for 35 percent of all AIDS-related deaths. And since many of them are not aware that they have HIV, they could be unknowingly
infecting others.
Various psychological barriers may be keeping this older at-risk population from getting tested. Among them are a general mistrust of the government - for example, the belief that the government is run by a few big interests looking out for themselves - and AIDS-related conspiracy theories, including, for example, the belief that the virus is man-made and was created to kill certain groups of people.
Now, a team of UCLA-led researchers has demonstrated that government mistrust and conspiracy fears are deeply ingrained in this vulnerable group and that these concerns often - but in one surprising twist, not always - deter these individuals from getting tested for HIV. The findings are published Jan. 29 in the peer-reviewed journal The Gerontologist.
"Our work suggests that general mistrust of the government may adversely impact peoples' willingness to get tested for HIV/AIDS," said Chandra Ford, an assistant professor of community health sciences at the UCLA Fielding School of Public Health and the study's primary investigator. "HIV/AIDS is increasing among people 50 and older, but there's not a lot of attention being paid to the HIV-prevention needs of these folks. Older adults are more likely to be diagnosed only after they've been sick, and as a result, they have worse prognoses than younger HIV-positive people do.
"Also, the CDC recommends that anyone who's in a high-risk category should be tested every single year," she said. "These findings mean that the CDC recommendations are not being followed." The researchers sought to test the association between mistrust of the government, belief in AIDS conspiracy theories and having been tested for HIV in the previous year. For the cross-sectional study, they worked with data from 226 participants ranging in age from 50 to 85. Participants were recruited from three types of public health venues that serve at-risk populations: STD clinics, needle-exchange sites and Latino health clinics. Of the participants, 46.5 percent were Hispanic, 25.2 percent were non-Hispanic blacks, 18.1 percent were non-Hispanic whites and 10.2 percent were of other races or ethnicities. The data were collected between August 2006 and May 2007.
The researchers found that 72 percent of the participants did not trust the government, 30 percent reported a belief in AIDS conspiracy theories and 45 percent had not taken an HIV test in the prior 12 months. The more strongly participants mistrusted the government, the less likely they were to have been tested for HIV in the prior 12 months.
Several of the findings surprised the researchers - for example, the fact that HIV testing rates among this population were not higher at the locations where the participants were recruited, given that these locations attract large numbers of people with HIV. "This finding is concerning because the venues all provide HIV testing and care right there," Ford said.
And there was an even bigger, perhaps counterintuitive surprise. The more strongly participants believed in AIDS conspiracy theories, the more likely they were to have been tested in the previous 12 months.
"We believe they might be proactively testing because they believe it can help them avoid the threats to personal safety that are described in many AIDS conspiracies," Ford said. "For instance, if I hold these conspiracy beliefs and a doctor tells me I tested negative, I might get tested again just to confirm that the result really is negative."
By contrast, individuals who reported mistrusting the government may not have been tested because the venues where they were recruited were, in fact, government entities, Ford said.
The study has some weaknesses. For instance, the study design did not allow the researchers to determine whether the participants held their beliefs before or after being tested; thus, the researchers couldn't tell what prompted their mistrust of the government or conspiracy beliefs. Also, it's possible that the prevalence of these theories is higher in this group than it is in the general public and that some participants may have been afraid to tell the truth.
The next step in the research is to study other groups of older adults to determine if these views are more widely held than just among the at-risk population the researchers studied.
Steven P. Wallace, Sung-Jae Lee and William Cunningham, all of UCLA, and Peter A. Newman of the University of Toronto co-authored the study.
The National Institute of Mental Health (5 RO1 MH069087, 5K01MH085503, R34MH089719); the UCLA Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME), under a grant from the National Institute on Aging (P30-AG02-1684); the UCLA AIDS Institute; the UCLA Center for AIDS Research (CFAR); the California Center for Population Research (5R24HD041022); and the National Institute on Drug Abuse (R01 DA030781) funded this study.
The Resource Centers for Minority Aging Research Center for Health Improvement of the Elderly (RCMAR/CHIME) is part of the effort to reduce health disparities between minority and non-minority older adults. It does so by increasing the number of researchers who focus on the health of minority elders; enhancing the diversity in the professional workforce by mentoring minority academic researchers for careers in minority elders health research; improving recruitment and retention methods used to enlist minority elders in studies so that research can accurately identify and work toward solutions to health disparities; and creating culturally sensitive health measures that assess the health status of minority elders with greater precision and increase the effectiveness of interventions designed to improve their health and well-being. A central coordinating center provides logistical support to the RCMAR centers, facilitates communication and collaboration, and oversees issemination activities designed to reach the larger research and health professional communities, public policymakers and consumers. The coordinating center is also the national clearinghouse for measurement tools, instruments, publications, community activity, pilot research and other resources developed by RCMAR investigators.
The UCLA Fielding School of Public Health is dedicated to enhancing the public's health by conducting innovative research; training future leaders and health professionals; translating research into policy and practice; and serving local, national and international communities.
Faculty Referenced by this Article

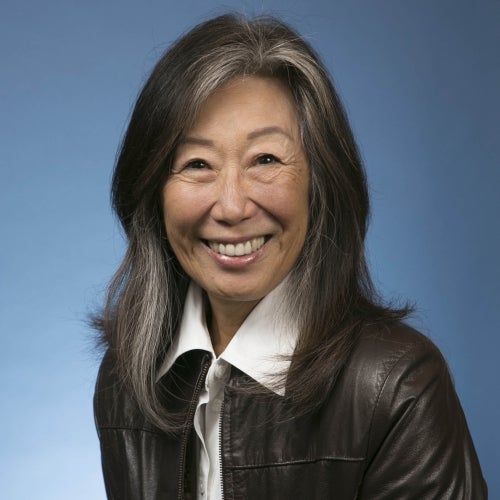
Professor of Community Health Sciences & Health Policy and Management, and Associate Dean for Research

Robert J. Kim-Farley, MD, MPH, is a Professor-in-Residence with joint appointments in the Departments of Epidemiology and Community Health Sciences

Assistant Dean for Research & Adjunct Associate Professor of Community Health Sciences

Director of Field Studies and Applied Professional Training