The U.S. lags in life expectancy, even while spending more than any wealthy country in the world
A research team led by UCLA FSPH faculty found as much as $1.9 trillion of financial waste in the current U.S. healthcare system.

A team jointly led by UCLA Fielding School of Public Health researchers has found the United States fall well behind other countries in life expectancy, while spending the most money on healthcare – nearly twice as much per capita – as other wealthy countries.
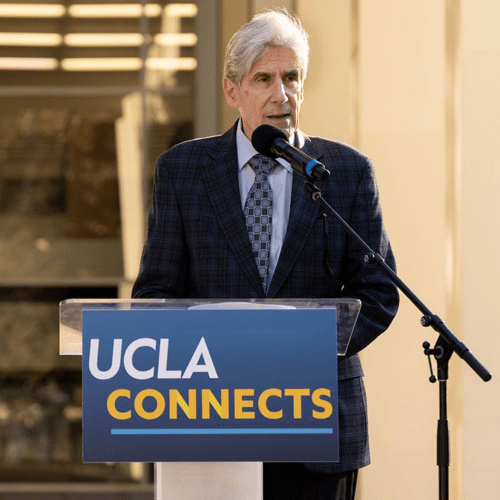
“Considering what we get – life expectancy for the dollars spent – do we spend the money in the right places?” asked Dr. Jonathan Fielding, UCLA FSPH distinguished professor of health policy and management and co-author of research published today by the American Journal of Public Health (AJPH). “The answer is no. We spend more, get less, and waste more than every other wealthy country in the world, and administrative costs, fraud and excessive prices do not add anything to a better life.”
Researchers found that depending on the category and type of spending, estimates of the financial waste in the U.S. range from $600 billion to more than $1.9 trillion per year, or roughly $1,800 to $5,700 per American annually. If saved, those amounts could fund huge increases in medical research, disease prevention, food assistance, universal child care, paid family leave, free college tuition and pre-K across the nation, and even a $238 billion middle class tax cut.
“The plot of the current public’s health story, that more healthcare is always better and more expensive is always better, is out of focus. We need a better plot,” said Dr. Steven Teutsch, professor of health policy and management at UCLA FSPH and former director of prevention research at the U.S. Centers for Disease Control and Prevention. “Good public health and population health approaches and strategies can add more years of life than can medical care, and every wasted dollar in healthcare is one less dollar for public health, schools, jobs, housing, and parks.”
The research was made available this week in a special edition of the peer-reviewed journal, published by the American Public Health Association. The interdisciplinary research team includes scholars from 12 universities and institutions, including Arizona State University, Columbia University, Cornell University, George Washington University, the University of Minnesota, the University of Wisconsin, and UCLA. Co-authors include Frederick Zimmerman, UCLA FSPH professor of health policy and management.
The special section includes peer-reviewed research and analysis, as well as editorials outlining issues, potential policy changes, and possible paths forward. These elements include an analysis of opportunity costs, defined as the potential benefits lost when choosing one alternative over another. Because by definition they are unseen, opportunity costs can be easily overlooked, but understanding the potential missed opportunities foregone by choosing one investment over another allows for better decision-making. Among the possibilities suggested by the analysis, which would all be covered by the larger, $1.9 billion estimate, are:
- Tripling the annual National Institutes of Health (NIH) research budget ($117.6 billion), and the annual budget for research and development (R&D) of the U.S. biopharmaceutical sector ($71.4 billion);
- Total annual direct and indirect costs of diagnosed diabetes in the U.S. ($245 billion), and the annual estimated costs of the American Housing and Economic Mobility Act ($50 billion);
- Annual estimated costs associated with switching to 100% renewable energy in the U.S. ($423.9 billion);
- Universal child care ($42 billion), paid family leave ($28 billion), and double the budget of the Supplemental Nutrition Assistance Program (SNAP) ($68 billion);
- Free annual tuition across all public U.S. colleges and universities ($79 billion), and free annual universal Pre-K ($26 billion), and
- Repeal of the estate tax ($64 billion), and a 10% tax reduction to those earning under $200,000 ($174 billion)
These numbers, and options, should make it clear what is at stake absent change, experts said.
“Rising per capita clinical care costs erodes federal, state, and family budgets,” said Mac McCullough, an Arizona State University health economist and co-author of the research. “And it means that less money is available for investments in other determinants of health, including education, job development, housing, environmental issues, as well as necessary infrastructure such as public health—all factors that contribute to better life expectancy in a population.”
In 2018, national health expenditures (NHE) in the U.S. grew to $3.6 trillion, nearly 18% of the Gross Domestic Product (GDP). The U.S. spends nearly twice as much per capita as other high income countries, but mounting evidence demonstrates that a significant amount of American medical care spending does little or nothing to improve population-wide health outcomes - and is therefore wasteful, the researchers found.
In life expectancy at birth, for example, based on 2019 figures, the U.S. reported 78.7 years; the equivalent in Canada, France, and the United Kingdom was 79, while Australia, Ireland, New Zealand, Spain, and Sweden reported 80, and Japan, Italy, Norway, and Switzerland all reported 81. In infant mortality, the U.S. reported 5.8 deaths per 1,000 live births; Canada reported 4.7, the United Kingdom 3.9, France 3.8, Australia 3.1, Sweden 2, and Japan 1.9. U.S. rates by state varied widely, from 3.6 in New Hampshire, 3.9 in New Jersey, and 4.2 in California, Connecticut, and Massachusetts, to 7.1 in Oklahoma and West Virginia, 7.2 in South Carolina, 7.5 in Arkansas, 7.6 in Louisiana, and 8.3 in Mississippi.
Significantly, the current COVID-19 pandemic has made clear the burdens the current wasteful system puts on low-income and minority groups, as shown by demonstrated shortfalls in health equity measurements, defined as “the absence of avoidable, unfair, or remediable differences among groups of people,” which in turn, imposes excess costs on individual Americans, as well as the U.S. in comparison to the country’s economic competitors.
“The pandemic is forcing a national reckoning over the disproportionate coronavirus-related illness and death in communities of color and other inequities that persist in this nation,” said Dr. Dora L. Hughes, professor at The George Washington University and a former senior advisor with the U.S. Department of Health and Human Services. “Because of this waste, we do not have additional dollars for investments to improve equity, especially in the first years of life, and we put ourselves at a disadvantage in economic competitiveness: our ability to thrive as a nation.”
The researchers broke down the types of waste as follow:
- Administrative Waste
- Excessive Prices
- Fraud and Abuse
- Missed Prevention Opportunities
- Overuse of Clinical Services
- Clinical Inefficiencies
Specific dollar values, as determined through a variety of studies, methods, and categories, are provided in Tables A1 to A7 of the analytic essay “Excess Medical Care Spending: The Categories, Magnitude, and Opportunity Costs of Wasteful Spending in the U.S.” Teutsch noted that several of these categories (administrative waste, prices, fraud and abuse) do not involve any change in clinical services.
The issue of medical waste is not new, of course; in 2012, the National Academies of Sciences, Engineering and Medicine (NASEM) published For the Public’s Health: Investing in a Healthier Future, an analytical report by the Institute of Medicine (IoM), now an element of NASEM. Recommendation #1 in the report, setting national targets for life expectancy and per capita medical care costs was recommended because linkage between these two is clear.
“The opportunity cost of a poorly performing, overly expensive healthcare system is detrimental to public health,” said Dr. Marthe Gold, chair of the 2012 effort, a senior scholar with the New York Academy of Medicine, and a contributor to the work published this week in the AJPH. “Traditional approaches to reducing healthcare spending will not enable the U.S. to achieve parity with high-resource nations; strategies to eliminate waste and reduce the demand for low-value healthcare are essential.”
The impact, and causes, of these realities, are illustrated by the idea of an inverted “U,” where additional medical care costs actually decreases life expectancy, authors said.
“Continuously increasing healthcare prices and consequent increase in healthcare expenditures has crowded out spending on public health and important social determinants,” said co-author Dr. Sanne Magnan, with HealthPartners Institute and the University of Minnesota School of Medicine. “Excess healthcare prices reduce resources available to invest in public health and other drivers of health and well-being.”
Sponsorship and Funding: This work was done under the auspices Health Care Expenditures Collaborative from the National Academies of Sciences, Engineering and Medicine. Support was provided by the authors’ institutions.
Data Availability Statement: All relevant data are available via the American Public Health Association.
Citation: Magnan, Sanne; Teutsch, Steven; et al, (2020), AJPH Special Section: “Changing the Public’s Health Story: Reducing Wasteful Medical Care Spending,” etc., American Journal of Public Health, AJPH-202033002
The UCLA Fielding School of Public Health, founded in 1961, is dedicated to enhancing the public's health by conducting innovative research, training future leaders and health professionals from diverse backgrounds, translating research into policy and practice, and serving our local communities and the communities of the nation and the world. The school has 690 students from 25 nations engaged in carrying out the vision of building healthy futures in greater Los Angeles, California, the nation and the world.
Faculty Referenced by this Article

Dr. Ron Andersen is the Wasserman Professor Emeritus in the UCLA Departments of Health Policy and Management.

EMPH Academic Program Director with expertise in healthcare marketing, finance, and reproductive health policy, teaching in the EMPH, MPH, MHA program
Nationally recognized health services researcher and sociomedical scientist with 25+ years' experience in effectiveness and implementation research.

Professor of Community Health Sciences & Health Policy and Management, and Associate Dean for Research

Dr. Michelle S. Keller is a health services researcher whose research focuses on the use and prescribing of high-risk medications.