Report: Medi-Cal patients with complex needs experienced some improvement with the Health Homes Program
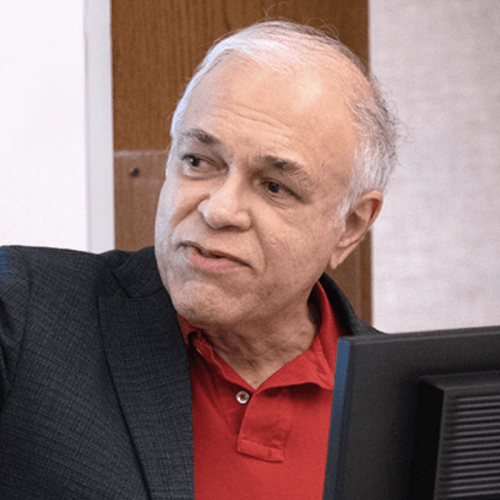
A team led by Dr. Nadereh Pourat has found that Medi-Cal patients with complex needs experienced improvements in some health-related outcomes.

Researchers at the UCLA Fielding School of Public Health's UCLA Center for Health Policy Research (CHPR) have released findings from the second Health Homes Program (HHP) Interim Evaluation report. The report, created by the Health Economics and Evaluation Research Program team at UCLA CHPR and led by Dr. Nadereh Pourat, UCLA Fielding School of Public Health professor of health policy and management, provides updates on program participants’ enrollment patterns, demographics, and services received that were reported in the first interim evaluation report.
Additionally, this report includes analyses of changes in HHP core metrics, health care utilization, and estimated Medi-Cal payment measures compared to a control group, or a group of patients with similar complex needs not enrolled in HHP, said Pourat, who also serves as associate director at CHPR.
HHP was implemented by the California Department of Health Care Services (DHCS) with the overarching goal to attain the “Triple Aim” quality improvement initiative of achieving better health outcomes and lowering health care costs. As of September 30, 2020, the program served 48,925 Managed Care Plan (MCP) beneficiaries with complex needs, including individuals with chronic health and/or mental health needs, as well as individuals experiencing homelessness. Extra services were provided at no cost to Medi-Cal members, and provided through care coordination, which as previous studies have shown, may be key to reducing avoidable health care costs.
The UCLA CHPR research team was selected to lead the program’s evaluation efforts, along with other California DHCS Medicaid 1115 Waiver programs such as the Whole Person Care (WPC) and the Public Hospital Redesign and Incentives in Medi-Cal (PRIME) Program.
“The Health Homes Program interim report findings show some promising improvements in how the program impacted service use, and will certainly help inform programs that serve patients who can benefit from various medical and social support services,” Pourat said. “These robust programs are vital in improving health care delivery and reducing cost expenditures.”
Additional features of the second report include the categorization of enrollees based on their use of the emergency departments and hospitals prior to program enrollment. The enrollee population consisted of 6% with super utilization (14.9 emergency department visits and 4.1 hospitalizations on average per year) and 35% with moderate utilization (2.7 emergency department visits and 0.5 hospitalizations on average per year). The report also included analyses of changes in the program’s core metrics, health care utilization, and estimated Medi-Cal payment measures compared to a group of Medi-Cal beneficiaries resembling HHP enrollees, but not enrolled in the program.
The findings indicated some improvements in emergency department and hospital utilization, access to needed outpatient services, screening for depression and follow-up, and overall estimated Medi-Cal payments. For example, HHP enrollees had 19 fewer ED visits and 10 fewer hospitalizations per 1,000 months every 6 months during the program, which were significant declines compared to before HHP and compared to the control group. Other measures that reflected care processes and health outcomes show no significant change after the first year of enrollment. A future report will assess health outcomes beyond the first year of enrollment.
Other report findings include:
- Of the 48,925 individuals enrolled in HHP between July 1, 2018, and September 30, 2020, 38,228 were enrolled under state plan amendment (SPA) 1 for enrollees with chronic physical health conditions or substance use disorders and 10,697 were enrolled under SPA 2 for enrollees with severe mental illness.
- MCPs reported that they had developed program delivery networks with 244 unique Community-Based Care Management Entities (CB-CMEs) by September 2020. These entities were primarily community health centers (41%).
- The majority of HHP enrollees were 50–64 years old (50%), women (59%), and spoke English as their primary language (72%). Nearly half of enrollees were Latinx (46%).
- Prior to enrollment, the most common chronic conditions among SPA 1 enrollees were hypertension (71%) and diabetes (54%). The most common condition among SPA 2 enrollees was depression (72%).
- For HHP enrollees, rates of outpatient services increased in the first six months after enrollment and then declined, but rates remained above those levels seen prior to enrollment.
- Estimated Medi-Cal payments increased as a slower rate for both SPA 1 and SPA 2 HHP enrollees compared to the control group.
HHP was authorized under California Assembly Bill 361 and approved by the Centers for Medicare and Medicaid Services under Section 2703 of the 2010 Patient Protection and Affordable Care Act. It is operated in 12 California counties by 16 MCPs that contract with CB-CMEs or directly provide services to HHP enrollees. The evaluation efforts are supported by the generous contribution of The California Endowment.
by Elaiza Torralba
The UCLA Fielding School of Public Health, founded in 1961, is dedicated to enhancing the public's health by conducting innovative research, training future leaders and health professionals from diverse backgrounds, translating research into policy and practice, and serving our local communities and the communities of the nation and the world. The school has 761 students from 26 nations engaged in carrying out the vision of building healthy futures in greater Los Angeles, California, the nation and the world.
Faculty Referenced by this Article

Dr. Michelle S. Keller is a health services researcher whose research focuses on the use and prescribing of high-risk medications.

EMPH Academic Program Director with expertise in healthcare marketing, finance, and reproductive health policy, teaching in the EMPH, MPH, MHA program

Professor of Community Health Sciences & Health Policy and Management, and Associate Dean for Research

Dr. Ron Andersen is the Wasserman Professor Emeritus in the UCLA Departments of Health Policy and Management.
Nationally recognized health services researcher and sociomedical scientist with 25+ years' experience in effectiveness and implementation research.