Conservatorships can result in a ‘bottleneck’ effect in psychiatric hospitals
UCLA researchers found that conservatorships result in psychiatric hospitalizations due to a lack of permanent housing & community-based treatment.

At a time when public and private agencies and the legal system are grappling with how to best assist people who live at the intersection of homelessness and mental illness during a global pandemic, UCLA researchers have found mental health conservatorships for people with disabling, severe mental illness who are also homeless can result in lengthy psychiatric hospitalizations.
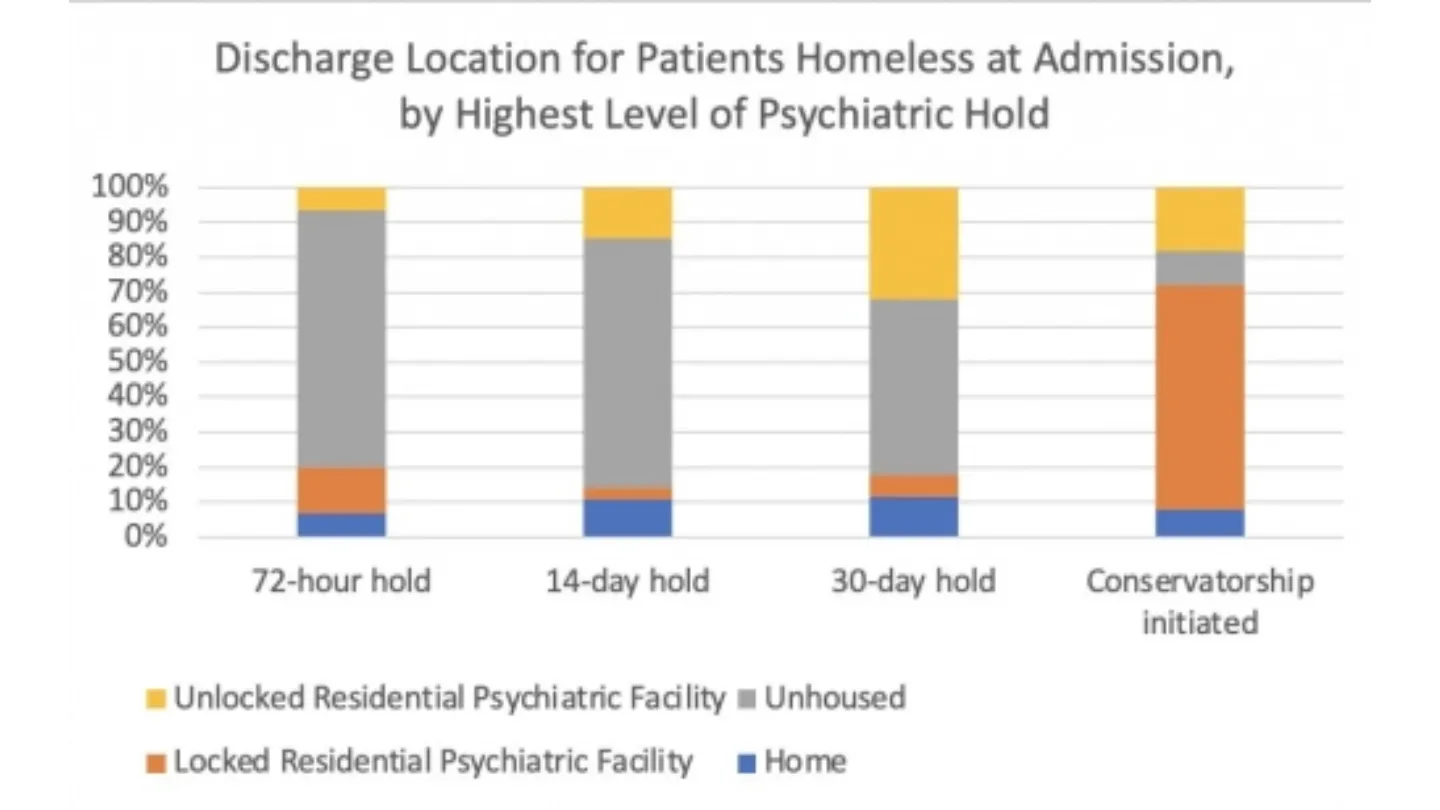
“Our study found that mental health conservatorships resulted in very lengthy inpatient stays for those who were homeless when conserved, sometimes as long as months or even a year,” said Dr. Kristen Choi, UCLA Fielding School of Public Health assistant professor of health policy and management. “We observed a ‘bottleneck’ effect in this study. There are very few long-term housing options for people who are disabled by mental illness and in need of supportive housing in Los Angeles. When these individuals are stabilized and ready for a lower level of community-based care, there is no place for them to go.”
Choi, a psychiatric nurse who is also an assistant professor with the UCLA School of Nursing, led the current study, “Mental Health Conservatorship Among Homeless People With Serious Mental Illness.” Mental health conservatorships, known as a Lanterman-Petris-Short Act (LPS) Conservatorship in California, are highly restrictive and thus reserved only for individuals with severe, ongoing disability from mental illness who cannot accept voluntary treatment. There is a strict legal process for initiating such conservatorships that involves review and monitoring by the courts.
“It is important to note that the majority of people experiencing homelessness do not have mental illness,” said Dr. Enrico Castillo, a psychiatrist with the UCLA Center for Social Medicine and Humanities. “Homelessness is not the same thing as mental illness and as such, the solution to homelessness is housing, not psychiatric treatment.”
The most recent measurement, the 2020 Greater Los Angeles Homeless Count, found 66,436 people in Los Angeles County experiencing homelessness; the 2021 survey was suspended because of the COVID-19 pandemic. At the same time, across the United States, the best available estimate of homelessness is some 580,466 people, according to the U.S. Department of Housing and Urban Development. Twenty-one percent of individuals who are homeless have serious mental illness, compared with 5 percent in the general U.S. population. Mental illness among people who are homeless is associated with higher risk for mortality, disability, substance use disorders, and suicide.
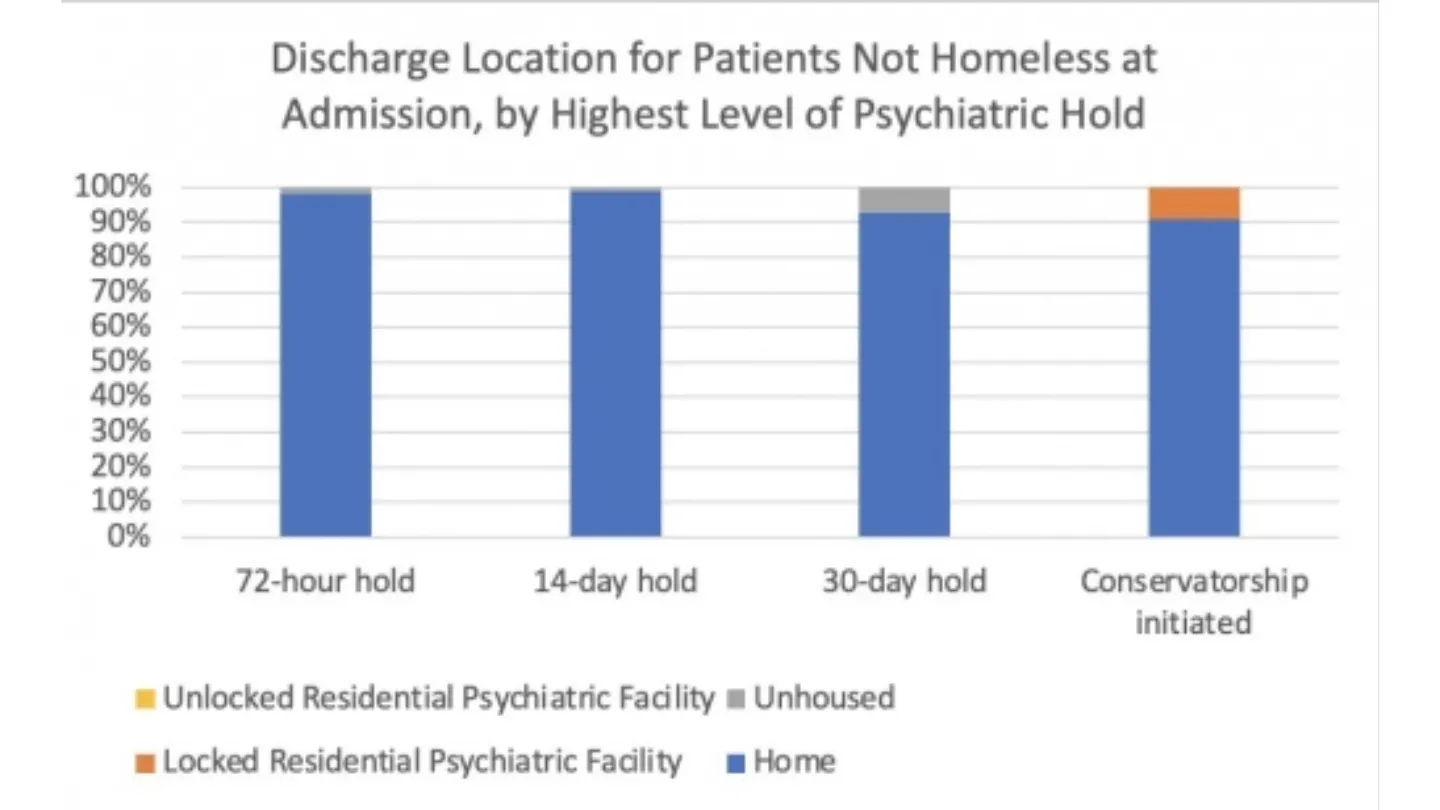
Publication of the study is pending in an upcoming edition of the peer-reviewed journal Psychiatric Services, published by the American Psychiatric Association. It is currently available on-line. The researchers from the UCLA Fielding School and the UCLA Center for Social Medicine and Humanities examined a sample of 795 adults, 18 years of age or older, who were hospitalized on an involuntary psychiatric hold in Los Angeles between 2016 and 2018. They examined discharge and mental health conservatorship outcomes for patients who were homeless. The researchers found that inpatient stays were almost four weeks longer for individuals who were homeless when admitted compared to those who were housed.
“For the minority of people experiencing homelessness who also have severe and disabling mental illness, such as those in our study, supportive housing options that combine treatment with housing are greatly needed in Los Angeles,” said Dr. Marissa Seamans, a UCLA Fielding School assistant professor of epidemiology and a co-author.
The study was conducted in partnership with Gateways Hospital and Mental Health Center, a safety net mental health system in Echo Park that aims provides mental health care to all people regardless of their ability to pay. In response to their growing homeless patient population and the results of this study, Gateways Hospital has formed a new partnership with the Homeless Outreach and Mobile Engagement (HOME) Team pilot program to link street-based psychiatric treatment with inpatient, outpatient, and residential treatment in the Gateways system.
“This partnership will enable us to better meet the needs of homeless individuals who are living in the streets due to their mental health related impairments,” said Dr. Shayan Rab, a street psychiatrist with the HOME Team. “Street-based mental health services can be a first step in addressing long-term treatment needs. At the same time, more residential treatment options in Los Angeles is ultimately the solution we need most.”
Methods: This observational study used administrative data from a safety-net psychiatric hospital in Los Angeles. The sample included 795 adults, 18 years of age or older, who were hospitalized on an involuntary psychiatric hold between 2016 and 2018.
Funding: This work was supported by the UCLA School of Nursing, and was conducted in partnership with Gateways Hospital and Mental Health Center. The authors report no financial relationships with commercial interests.
Data availability statement: Inquiries about the data presented in this study should be directed to the corresponding author, Dr. Kristen Choi at krchoi@ucla.edu.
Citation: Kristen R. Choi, Enrico G. Castillo, Marissa J. Seamans, Joseph H. Grotts, Shayan Rab, Ippolytos Kalofonos, Meredith Mead, Imani J. Walker, and Sarah L. Starks. Mental Health Conservatorship Among Homeless People With Serious Mental Illness. Psychiatric Services, October 2021. https://doi.org/10.1176/appi.ps.202100254
The UCLA Fielding School of Public Health, founded in 1961, is dedicated to enhancing the public's health by conducting innovative research, training future leaders and health professionals from diverse backgrounds, translating research into policy and practice, and serving our local communities and the communities of the nation and the world. The school has 761 students from 26 nations engaged in carrying out the vision of building healthy futures in greater Los Angeles, California, the nation and the world.
Faculty Referenced by this Article

Dr. Joseph Davey is an infectious disease epidemiologist with over 20 years' experience leading research on HIV/STI services for women and children.

Professor of Community Health Sciences & Health Policy and Management, and Associate Dean for Research

Dr. Ron Andersen is the Wasserman Professor Emeritus in the UCLA Departments of Health Policy and Management.

EMPH Academic Program Director with expertise in healthcare marketing, finance, and reproductive health policy, teaching in the EMPH, MPH, MHA program

Dr. Anne Rimoin is a Professor of Epidemiology and holds the Gordon–Levin Endowed Chair in Infectious Diseases and Public Health.

Robert J. Kim-Farley, MD, MPH, is a Professor-in-Residence with joint appointments in the Departments of Epidemiology and Community Health Sciences

Dr. Michelle S. Keller is a health services researcher whose research focuses on the use and prescribing of high-risk medications.
Nationally recognized health services researcher and sociomedical scientist with 25+ years' experience in effectiveness and implementation research.